Correspondence
Sir
A segmental white patch on skin is a common cosmetic
concern among Indians, where differentiation between
different types and causes of depigmentation is
challenging. Segmental vitiligo is an acquired autoimmune
condition causing unilateral chalky-white patches on the
skin presenting a band-shaped distribution.[1]
Nevus depigmentosus (ND) is classically defined as a
congenital nonprogressive, depigmented macule with
serrated borders, which is mostly unilateral in distribution.[2]
An adolescent man presented to the outpatient department
with a complaint of a depigmented lesion over the left side
of his face for 6 years showing no regression/ advancement
in the last 6 years [Figure 1]. By studying the relevant
history and on evaluation, a diagnosis of segmental
vitiligo was made and the patient was offered a myriad of
treatment options. Doctor and patient conclusively made
the decision to go for surgical treatment and minipunch
grafting was planned.
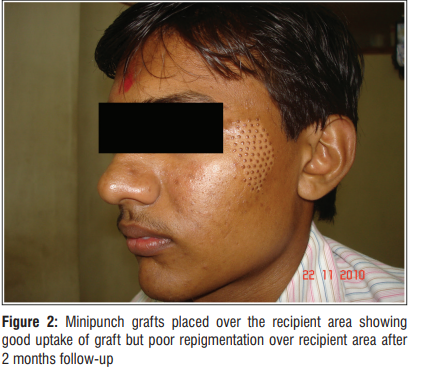
The grafts were extracted from the donor site (behind the
ear) using 1.5mm sized punch, and then placed over the
recipient site and fixed using cyanoacrylate glue [Figure 2].

The patient was followed up every week for the first
month after surgery, and thereafter every fortnightly.
After 4 months post-op, it came to the authors’
notice that although the graft “take-up” was proper,
the repigmentation around it had not even begun
slightly, although adequate treatment with daily
psoralen and solar UVA (PUVAsol) therapy was
provided.
Upon reevaluating the case, the patient confessed that
the depigmented lesion was in fact present since birth.
This prompted the author to change the diagnoses to
ND for which the suitable surgical option would be split
thickness skin graft (STSG) or noncultured epidermal cell
suspension (NCES).[3]
The difficulty was to provide sufficient color matching
by performing one of these two surgeries while the
minipunch grafts were still in place. To eliminate the risk
of cobblestoning and mismatching altogether the author
decided to remove the “in place” grafts by a similar
process using 1.5 mm sized punch [Figure 3], following
which the recipient area was given a rest period to heal
for 8 weeks.
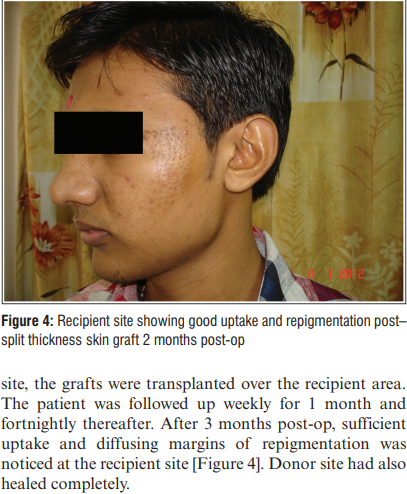
On the next follow-up, STSG surgery was planned for the
patient, which is also considered the surgery of choice for
ND.[3]
2 x 2cm sized STSG were taken from the anterolateral
aspect of right thigh; after derma abrading the recipient

This case helped us review different surgical methods
for the treatment of ND. Kim and Park[4]
observed
that suction-blister grafting provided satisfactory
repigmentation in case of ND, whereas Olsson and Juhlin[5]
observed no repigmentation when treated by transplant of
a melanocyte-rich cell-suspension. Minipunch grafting,
however, has been proved to be of little to no significance
in ND according to past literature, which is also in
concordance with the results observed in our case.
In conclusion, thorough history taking is always a
doctor’s best friend and a dermatosurgeon should never
shy from taking a “U-TURN” approach in today’s times
of uncertainty for the greater good of the patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate
patient consent forms. In the form the patient(s) has/have
given his/her/their consent for his/her/their images and
other clinical information to be reported in the journal.
The patients understand that their names and initials will
not be published and due efforts will be made to conceal
their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Yogesh M. Bhingradia, Heena B. Singdia1 , Akshay A. Vetal2
Shivani Skin and Cosmetic Clinic, Surat, Gujarat,
1
Department of Skin and VD, SMS Medical College Jaipur, Jaipur, Rajasthan, 2
Department of Skin and VD, LTMC SION Hospital, Mumbai, Maharashtra, India
Address for correspondence
: Dr. Yogesh M. Bhingradia,
Shivani Skin and Cosmetic Clinic, Surat 395006, Gujarat.
E-mail: yogeshbhingradia@gmail.com
References
- Sharquie KE, Noaimi AA, Salmo HM. Pityriasis alba versus vitiligo.
Journal of the Saudi Society of Dermatology & Dermatologic
Surgery 2013;17:51-4. - Kim SK, Kang HY, Lee ES, Kim YC. Clinical and histopathologic
characteristics of nevus depigmentosus. J Am Acad Dermatol
2006;55:423-8. - Gupta S, Goel A. Letter to the editor: Nevus depigmentosus needs
transplant of epidermal sheets. Dermatol Surg 2005;31:1746-7 - Kim DY, Park YK, Hann SK. Recurrence of nevus depigmentosus
after an autologous epidermal graft. J Am Acad Dermatol
2008;58:527-9 - Olsson MJ, Juhlin L. Leucoderma treated by transplantation of a
basal cell layer enriched suspension. Br J Dermatol 1998;138:644-8
This is an open access journal, and articles are distributed under the terms of the
Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows
others to remix, tweak, and build upon the work non-commercially, as long as
appropriate credit is given and the new creations are licensed under the identical terms.

How to cite this article: Bhingradia YM, Singdia HB, Vetal AA. Taking a “U- TURN” on the Road to Treating a Difficult Depigmented Lesion. J Cutan Aesthet Surg 0;0:0.


